To date, there is no effective drug for the treatment of Alzheimer’s disease. Currently available drug treatment options are limited to acetylcholinesterase inhibitors and memantines, each of which is used depending on the stage of the disease and directly affects the action of neurotransmitters in the brain. It is hard to believe, but these pharmacological approaches are still based on the findings of the 1970s and 1980s and show at best a short-term slowing of symptoms.
Worse, the clinical benefit of these widely prescribed antidementia drugs is now controversial, as the body can develop adaptive mechanisms and Alzheimer’s symptoms progress all the more rapidly when the drugs are discontinued.
But why have all pharmacological monocausal approaches failed so far?
As early as 2014, the U.S. neurologist Dr. Dale Bredesen correctly recognized that Alzheimer’s disease is a generalized metabolic disorder, i.e., a disease with a multitude of causes, which must also be addressed in their multitude in therapy, i.e., multimodal approaches must be pursued [1].
Bredesen explains the basis for reversibility as follows: Alzheimer’s disease does not arise because the brain does something it is not supposed to do, as is the case with cancer, for example. No, Alzheimer’s is actually the consequence of an endogenous and thus also physiologically normal degradation program of the neurons and their interfaces, the synapses. But in Alzheimer’s disease, this ‘normal’ process, which is actually a protective function of our brain, has gone completely out of control, because the brain has been acutely stressed by numerous factors and is now desperately trying to protect itself.
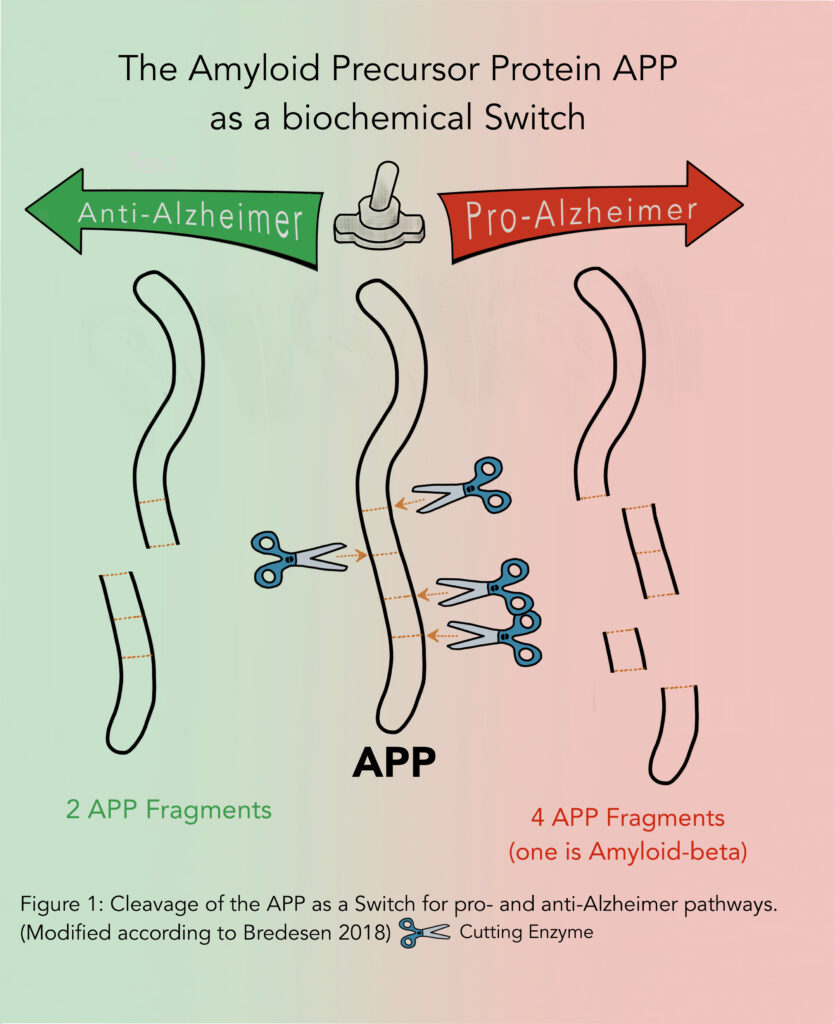
The scientific explanation starts with the so-called Amyloid Precursor Protein (APP), which is the ‘molecular switch’ for the anti- or pro-Alzheimer pathway (p. Figure 1). Which pathway is taken is determined by how often and at which site APP is cut. This cutting is done by enzymes called proteases, which can be thought of as molecular scissors.
If APP is cut once, and 2 fragments are formed, it goes in the Alzheimer-protective direction. This leads to the promotion of neuronal growth and the emergence of new synapses: new interconnections in the brain can now be formed. On the other hand, if APP is triple-cut, 4 fragments are formed, including amyloid-beta protein, a component of typical-Alzheimer’s plaques. The Alzheimer’s-promoting pathway is now in place: degradation of the neuronal network occurs, with loss of synapses and neurons. In Alzheimer’s disease, this natural balance between the anti- or pro-Alzheimer pathway becomes unbalanced in favor of the brain-damaging pathway. The challenge now is to stop this and restore the healthy balance.
But the good news is: Science now knows which risk factors drive the Alzheimer’s-promoting pathway at the APP interface (see Figure 1), and which promote the Alzheimer’s-protective processes. They must be identified in each patient – the former enhanced therapeutically, and the latter reduced or even eliminated. And this is what Bredesen has successfully done with his therapy program!
As an analogy, Bredesen uses the image of a leaky roof during rain to picture Alzheimer’s disease: there are up to 36 holes in the Alzheimer’s roof that need to be patched so that everything is tight again. Not every patient has the same holes, and therefore the protocol is customized based on the patient’s genetics, current health status and lifestyle.
Bredesen was able to implement these findings to his patient as well. In 2014, Bredesen’s therapy concept, called the ReCODE protocol (‘Reversal of Cognitive Decline’) was published in the scientific press for the first time. This novel therapy concept is a promising approach in the treatment of Alzheimer’s disease, as it follows a multifactorial strategy.
In the ReCode protocol, 6 different types of Alzheimer’s disease are defined according to the patient’s genetic variant of the ApoE gene (see genetics), predominant symptoms and co-existing diagnoses:
- Inflammatory (“hot”),
- Atrophic (“cold”),
- Glycotoxic (“sweet”),
- Toxic (“vile”),
- Vascular (“pale”) and
- Traumatic (“dazed”).
In this context, the specific type ultimately determines the therapeutic approach. The effect of each type-specific therapeutic strategy is assessed by a comprehensive cognitive examination, called a cognoscopy, using blood tests, genetic tests, microbiome tests, simple cognitive assessments, and imaging techniques.
The blood tests used in cognoscopy include numerous parameters. They can detect existing inflammations, current cell protection as well as the patient’s antioxidant capacity. Furthermore, metabolic disorders in the context of the metabolic syndrome are closely examined. A comprehensive analysis of the hormone status is carried out and also the cellular toxin/ heavy metal load mineral supply is examined.
The fact that the Bredesen method is actually effective and not an empty promise has now been proven in a large number of studies. In 2018, for example, Dr. Bredesen reported on 100 successfully treated patients in whom the symptoms of Alzheimer’s disease had already progressed to varying degrees, from mild to moderate cognitive impairment [2].
Through measures such as:
- Identification and treatment of pathogens,
- Repairing a permeable gut mucosa (“leaky gut”) and improving microbiome,
- Identification of insulin resistance and restoration of insulin sensitivity,
- Identification and correction of suboptimal nutrient, hormone, or neurotrophin (neurotrophins are endogenous signaling substances that cause targeted nerve cell connectivity; e.g.: BDNF),
- Identification of toxins and their elimination through detoxification,
He succeeded not only in slowing or halting the course of the disease, but also in improving symptoms!
However, it was also apparent in this study that the earlier the stage of the patient’s disease, i.e. the earlier the treatment took place, the better the therapeutic success. This is also a challenge, since Alzheimer’s disease, which can take decades to develop, is often diagnosed at an advanced stage when patients are no longer able to act.
Therapy strategy according to Dr. Nehls
Following Bredesen’s ReCode protocol, the German physician and molecular biologist Dr. Michael Nehls has also addressed the issue of ‘Alzheimer’s is curable’ in the book of the same name. Like Dr. Dale Bredesen, he points out that AD is a generalized metabolic disease, caused in particular by an unhealthy lifestyle, which can be counteracted equally by a healthy lifestyle.
His key messages include:
- Alzheimer’s is a deficiency disease;
- Alzheimer’s is preventable;
- Drugs cannot compensate for illness-causing deficiencies;
- Curative therapy is nevertheless possible.
Dr. Bredesen as well as Dr. Nehls have meanwhile published numerous books on this subject, which are aimed at the layman. They are helpful guides for those affected, patients at risk and their relatives, and provide valuable information so that you too can remain mentally fit for life!
The literature of Dr. Bredesen as well as of Dr. Nehls can be found under our book recommendations.
In addition, in our list of therapists you will find doctors & alternative practitioners who follow these treatment protocols.
Conclusion:
There is still no effective drug against Alzheimer’s disease, but with the multifactorial therapeutic approach of the U.S. neurologist Dr. Dale Bredesen, a treatment concept is finally available that enables individualized therapy for Alzheimer’s patients. This so-called ReCode protocol has been shown to halt the course of the disease and reverse symptoms in early-stage Alzheimer’s patients. This gives a lot of courage and hope and proves that Alzheimer’s disease is not an unavoidable fate! But do not forget: the earlier the treatment starts, the better the results. So the principle also applies to Alzheimer’s: better to act in time before it is too late!
References:
- DE Bredesen (2014) Reversal of cognitive decline: A novel therapeutic program. Aging, Vol 6, 9
- DE Bredesen et al (2018) Reversal of cognitive decline: 100 patients. J Alzheimers Dis Parkinsonism 8, 5
- DE Bredesen (2018) Die Alzheimer-Revolution. mvg-Verlag, ISBN 978-3-86882-900-6